Abstract
Amyloidosis is a protein deposition disorder wherein amyloid fibrils affect soft tissues and visceral organs. One subtype is light-chain (AL) amyloidosis, which is characterized by amyloidogenic immunoglobulins produced generally by clonal plasma cells. Kidney and heart are the most commonly involved organs by AL amyloidosis while liver and sensory/autonomic nervous system can be clinically prominent. In a minority, acquired Factor X (FX) deficiency (related to amyloid binding this factor) can provoke a profound bleeding diathesis.
We present a 62-year-old black male who was referred to our institution in May 2016 by a community hematologist after diagnoses of FX deficiency and monoclonal gammopathy. The patient initially presented with ecchymosis, hemearthroses, and blood per rectum. Workup revealed a hemoglobin 7.7g/dL, platelets 62x10³/µL and prolonged PT (35.4s) and aPTT (53.9s). Echocardiogram revealed concentric LV 'hypertrophy' and grade 2 diastolic dysfunction. Abdominal ultrasound identified an enlarged spleen of 18 cm. Fibrinogen level was 295mg/dL, PT and PTT mixing studies normalized, and FX activity was measured at 0.02U/mL (normal 0.2-0.4U/mL). Bone marrow biopsy showed plasma cell myeloma involving 50% of the marrow. He was started on therapy with cyclophosphamide, bortezomib, and dexamethasone.
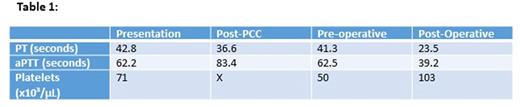
Unfortunately, the patient had no measurable response after 3 cycles of therapy at which time he presented with severe and progressive hemarthrosis, mucocutaneous bleeding, symptomatic anemia, thrombocytopenia, and elevations in PT/PTT. He received transfusions with fresh frozen plasma (FFP) around the clock, aminocaproic acid, and supportive transfusion of packed RBC and platelets. Due to active mucosal bleeding, the patient was administered vitamin K and transfused FFP every 4 hours. His coagulation parameters did not improve. Interestingly, despite his mixing studies correcting "in vitro," he failed to demonstrate any "in vivo" correction despite FFP transfusion and three plasmapheresis treatments. Given his refractory bleeding, the surgical service was consulted regarding the prospect of a splenectomy. In an effort to optimize the patient for surgery, he received prothrombin complex concentrate (PCC) without significant improvement (Table 1). Ultimately, the patient underwent splenectomy (estimated blood loss 200cc) and was managed intra-operatively with FFP and aminocaproic acid infusion. His coagulation studies and platelet count improved immediately post-operatively (Table 1), and repeat FX level the following day demonstrated a normal value of 0.48 U/mL. Surgical pathology of the spleen was consistent with extensive deposition of amyloid (lambda subtype). To date, the patient has had a complete normalization of coagulation studies and FX levels and is clinically responding to daratumumab therapy.
The incidence of coagulopathy in AL amyloidosis has been estimated to approach one third of all patients, largely due to acquired coagulation factor deficiency, and most commonly FX. Splenomegaly is present in fewer than 15% of patients with AL amyloidosis, however it is much more frequent in patients with acquired FX deficiency. Amyloid deposition in the spleen is thought to bind FX as well as sequesters platelets leading to potentially life threatening bleeding. Our review of the literature identified five previously reported cases of acquired FX deficiency secondary to AL amyloidosis which completely reversed after splenectomy (Kapoor et. al. American Journal of Hematology 2006), but our patient's presentation was particularly severe. Previous reports have also described the improvement of acquired FX deficiency in AL amyloidosis patients with high-dose melphalan (Choufani et. al. Blood 2001), although it is unclear what degree of clinically significant bleeding these patients were experiencing. Splenectomy is frequently reserved as last-line management in these patients, when more conservative measures such as FFP and plasmapheresis are not effective. This is due to the short half-life of the infused FX (Furie et. al. NEJM 1977), as well as its expedited clearance in the spleen, where it is bound to amyloid. While some cases using recombinant Factor VIIa and PCC have worked, they are more often ineffective. In patients with severe bleeding, splenectomy can produce rapid improvement as evidenced here.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal